Abstract

Background: Juvenile myelomonocytic leukemia (JMML) is a hematologic malignancy of infants and toddlers with both myelodysplastic and myeloproliferative features. The prognosis for patients (pts) with relapsed or refractory (r/r) JMML is poor and hematopoietic stem cell transplant (HCT) is the only curative therapy. The molecular hallmark of JMML is activation of the Ras/MAPK pathway. In preclinical studies, MEK inhibition was shown to be effective at reducing spleen sizes, restoring normal hematopoiesis, and extending survival compared to placebo in several genetically engineered mouse models of JMML. Trametinib is an orally bioavailable MEK1/2 inhibitor and is approved for treatment of several malignancies in adults. This Children's Oncology Group study (ADVL1521, NCT03190915) is the first clinical trial for pts with r/r JMML conducted in the United States. Pts are eligible if they have persistent clinical or molecular evidence of JMML after 1 cycle of high dose cytarabine, 2 cycles of a hypomethylating agent or HCT. Pts receive daily trametinib for up to 12 cycles (28 days) in the absence of disease progression or dose-limiting toxicity (DLT). Dosing is age-based with pts less than 6 years of age receiving 0.032mg/kg/day and those 6 years or older receiving 0.025mg/kg/day. An oral suspension is available for pts unable to swallow tablets. Using a Simon 2-stage design (10 pts in each stage), trametinib would be deemed effective if 3 or more pts achieved an objective response.
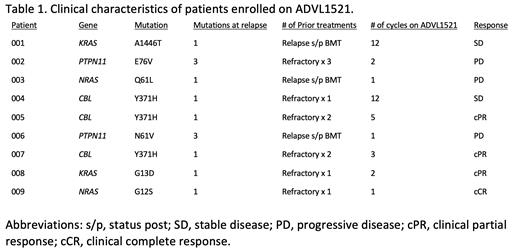
Results: From 2018-2021, 9 pts were enrolled; all 9 were eligible and evaluable for toxicity and response. Each pt had a detectable Ras mutation at the time of enrollment and was monitored for response using clinical and molecular criteria developed by an international consensus panel (Niemeyer et al, 2015). Five pts were less than 2 years of age. Three patients had relapsed post-HCT prior to enrolling and 6 patients were refractory to a median of 1.5 prior therapies (range 1-3). Four pts had an objective response (1 clinical complete response (cCR), 3 clinical partial responses, (cPR); 2 pts had stable disease and 3 had progressive disease (Table 1). Both pts with stable disease completed the maximum 12 cycles permitted on study. Two pts who achieved a cPR proceeded to HCT. One patient who achieved a cCR remains on study. No molecular responses were achieved. There were no dose-limiting toxicities; one pt had grade 4 thrombocytopenia probably related to trametinib. Of the 8 patients who consented to correlative studies, 7 had DNA methylation testing, 6 had kinome profiling, and 5 had RNASeq testing performed on both pre- and post-trametinib paired samples. DNA methylation testing revealed stable intrapatient methylation signatures across diagnostic, relapse and post-trametinib timepoints using the international consensus criteria (Schönung et al, 2020). Integrated kinome and RNASeq analysis revealed downregulation of proteins and genes involved in Ras/MAPK signaling.
Conclusions: In the first clinical trial for r/r JMML patients in the United States, 4 objective responses were observed among the initial 9 patients meeting the pre-defined criteria to deem trametinib effective. While clinical responses including resolution of splenomegaly, resolution of monocytosis and increased platelets counts were observed, no molecular responses were noted. The treatment of r/r JMML has historically depended on HCT. Recently, azacitidine has shown promise in treating r/r JMML. This trial demonstrates that trametinib is active in r/r JMML and has a favorable side effect profile. Ongoing analysis of extensive correlative testing results have revealed potential mechanisms of response and resistance to MEK inhibition. Future studies will focus on children with newly diagnosed JMML and combine trametinib with azacitidine with or without HCT.
Loh: MediSix therapeutics: Membership on an entity's Board of Directors or advisory committees. Barkauskas: Genentech: Current Employment.
Author notes
 This icon denotes a clinically relevant abstract
This icon denotes a clinically relevant abstract